Q. What is this life altering affliction?
A. The medical term and definition for this is dyspareunia= painful sexual intercourse, with no other discernible diagnosis (infection/neoplasm)
Q. What are some of the risk factors that might lead to dyspareunia?
A. Some of the reasons are:
-
- Vaginismus = involuntary contraction of some of the pelvic floor muscles (pubococcygeus) which can sadly make penetration almost impossible
- Vulvodynia / Vulvar Vestibulitis (pain occurring more generally and not during sex)
- Trauma (episiotomy/sexual assault)
- Surgery i.e. LEEP/LLETZ, lumbar spine operations
- Birth control & peri/post-menopausal (reduced oestrogen = thin/weak skin, reduced progesterone = reduced lubrication)
- Chronic urinary tract infections or bowel problems
- Autoimmune conditions i.e. fibromyalgia/Sjogrens/Diabetes = reduced lubrication
- Chronic hip/LSP pain
- Skin Conditions – Lichen Sclerosis, Lichen Planus, Eczema, Psoriasis
- Pelvic Inflammatory Disease (PID)
- Ovarian cysts
- Stress
- Being with the wrong partner?
- Sexual inexperience
Q. What are some of the symptoms associated?
A. Symptoms can include:
-
- Pain
- Burning
- Stinging
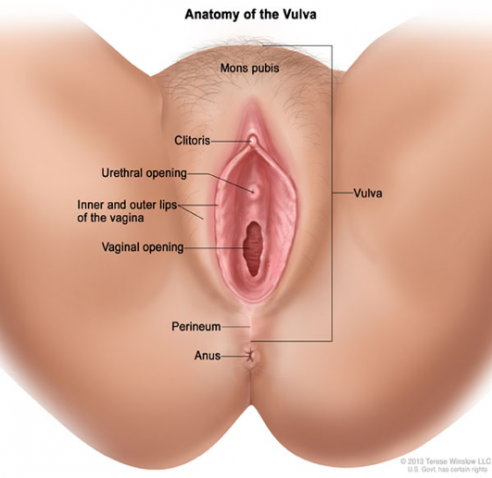
- Cramping of the vagina, clitoris or labia
These symptoms can occur during penetrative sex or after sexual intercourse has occurred. Symptoms can be felt deep inside the vagina, or superficial and close to the opening of the vagina.
Q. How common is dyspareunia?
A. It is very hard to estimate because many cases go unreported but some research has been done to determine this.
One study carried out on 200 women in Brazil showed that about 40% of women aged 40-65 experienced pain during sexual intercourse. In Scandinavia, a study of 3000 women showed that 13% of women aged 20-29 years and 6.5% for women aged 50-60 years reported symptoms. In America another study showed that 34% of women were affected and most of the women had not discussed their dyspareunia with a health care professional at all.
Q. What questions might an osteopath ask to guide your treatment?
A.
-
- When did your symptoms start?
- How long does the pain last for?
- Are the symptoms deep or more superficial?
- Does anything else aggravate these symptoms i.e. during your period or if you experience any irritable bowel syndrome?
- Has successful intercourse taken place previously?
- Have you tried lubrication and does this help?
- Are you breast feeding? This often leads to reduced lubrication because of the change in hormones.
Q. What Osteopathic studies have been done on women with dyspareunia?
A. A dissertation was carried out in 2012 in Spain for deep dyspareunia. It was a small study of 7 women. After treatment was completed, there was a very significant improvement in 5 of the women.
Osteopath Andrea Hoffman of Germany carried out research in 2005 which was published in Osteopathy Today. The study consisted of 28 women and concluded that Osteopathic treatment reduced pain significantly and greatly improved the quality of life for the women in the study.
Q. What might a Women’s Health trained Osteopath do for dyspareunia?
A. For any issues a patient presents with, osteopathy always aims to improve the following where necessary to begin with:
-
- Blood supply to the affected area as it is the blood that brings the healing properties to damaged tissues
- Drainage of the blood supply to the affected area, if blood gets in it also needs to get out easily otherwise a stagnation occurs and problems can be caused by that alone
- The nerve supply
- The lymphatics system that carefully carries away the waste in our bodies
- Balance of the skeleton, ligaments and muscles
The western medical model divides the body up into specific parts or organs, but the fact remains that no part of the body works independently. It is constantly interacting with it’s neighbours or other systems of the body.
We might, if necessary, then go on to do a very gentle and non-painful more in depth examination to try and locate where exactly the pain is originating. We may examine the fibrous centre of the perineum because of it’s influence on the pelvic floor, external genitalia, opening of the vagina and an internal examination of the vagina if relevant of:
-
- The pelvic floor muscles, to see if there is any tension or spasm from one side or the other
- The neck of the bladder
- The position and mobility of the cervix
- The ligaments to the cervix and uterus
In some cases it has been seen that simply an imbalance of the pelvic bones and the pelvic floor muscles has led to the cervix becoming pulled to one side and the lack of natural mobility of the cervix is lost, leading to the cervix becoming more rigid and a site of pain when touched directly during intercourse. This is of course a simple example but there are many different causes.
Whatever the reason, there is no need to suffer in silence with this because the effects of this can be absolutely devastating and sometimes completely unnecessary.
Claire Forrester, Registered Osteopath
M.Ost, PGDWHO, FMIH
The Form Practice
01954 214473

